Ever driven someplace and upon arrival wondered, “How did I get here?”
Ever been on a vacation, but 1 month later realized there were only a few fragments of memories from the get-away?
Ever had a moment of clarity, while sitting & waiting in a busy pain clinic for several hours, of “this can’t be ALL there is for me?”
Prevent Being Given The “Bean” Look!
Ever wake up thinking, “I don’t want to adult today!”?
Ever spend time to justify to yourself or someone else why you did X, Y or Z versus not what you know you were supposed to do?
Ever think back to how carefree and easy being a kid was?
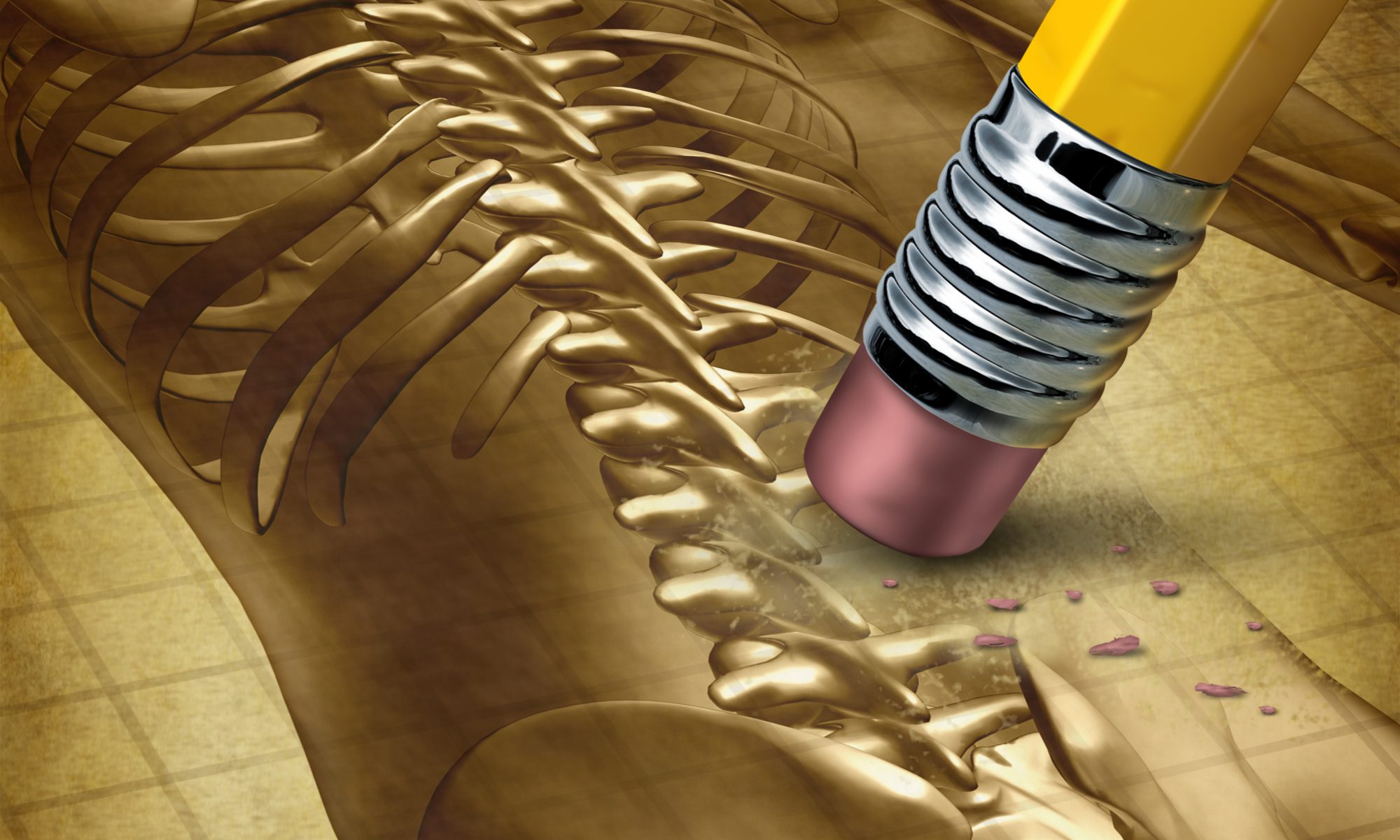
Continue reading “Prevent Being Given The “Bean” Look!”Is Degenerative Disc Disease Real?
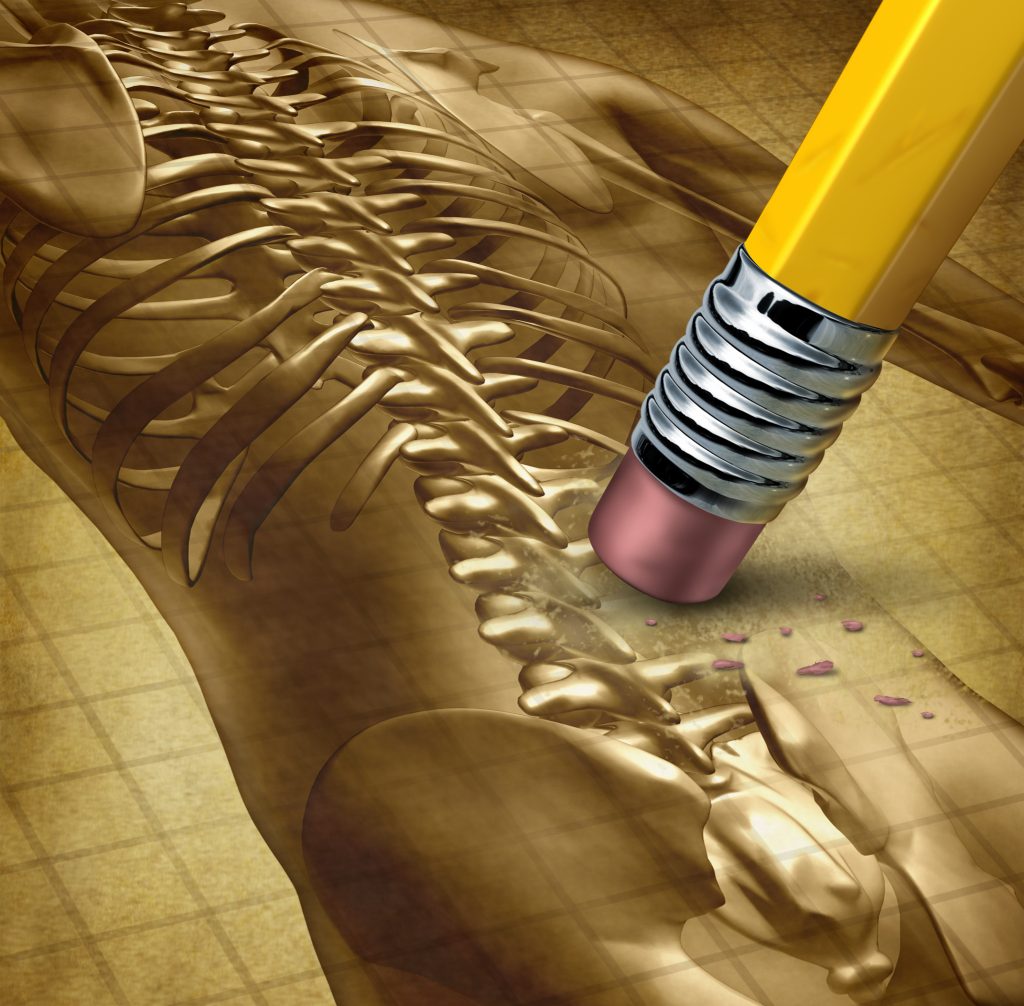
I was speaking with a client today who was recalling her appointment with a new pain management specialist. According to her, he was asking her about her medical history and back issues; to which she started listing off previous diagnoses such as Fibromyalgia, DDD/DJD (degenerative disc/joint disease), and spinal stenosis. At this point, he apparently became hostile with her and began a long diatribe about how DDD isn’t real and how he wished people would stop calling this a disease as it gives patients something to “whine about when there is actually nothing wrong with them!”
Continue reading “Is Degenerative Disc Disease Real?”Have You Been Stretching?
“Are you doing your stretching?” is always the question I ask my clients as they hobble into my office or when finding their hamstrings are like Golden Gate Bridge cables. However, this question should also asked by your PT, your massage therapist, your pain physiatrist, etc.
Continue reading “Have You Been Stretching?”The Hardest Thing to Change is Ourselves….
Change is hard and scary and sometimes downright daunting as it means we have to take a look at our lives and be willing to change. We know, need and want to live healthier. Maybe some of the changes you’re thinking of are to make some healthy changes to eating habits, start exercising again regularly, get more rest, or learn to use natural remedies instead of turning to over the counter medications for simple illnesses.
Continue reading “The Hardest Thing to Change is Ourselves….”Pain Relieving Essential Oils

Essential oils have been used for centuries to relieve a variety of conditions, pain and inflammation. Many essential oils have similar, and sometimes more effective, pain-relieving properties than many prescription or over-the-counter analgesics.
There are many benefits to using essential oils to get relief from pain and inflammation. For example, essential oils have fewer side effects than many modern drugs and they also help to soothe your mind and make you feel more relaxed. So, essential oils play an important role in pain management and in treating many inflammatory conditions.
If you suffer from chronic pain associated with arthritis, lower back pain, migraines, fibromyalgia, nerve pain or sciatica, then essential oils are excellent home remedies to treat the pain.
Continue reading “Pain Relieving Essential Oils”Understanding Blood Pressure
Healthy and unhealthy blood pressure ranges
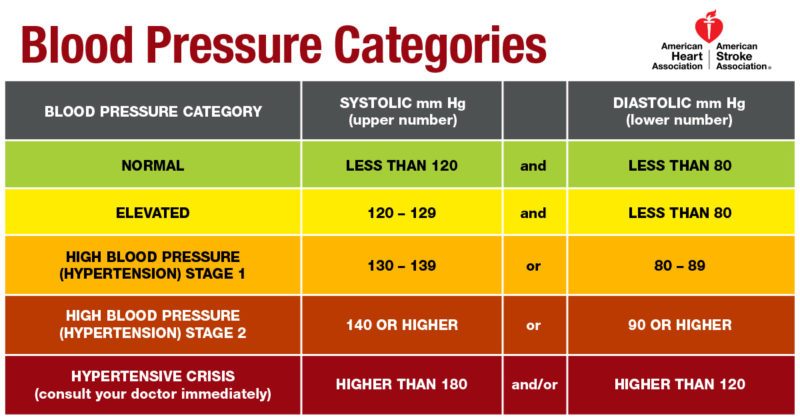
Learn what’s considered normal, as recommended by the American Heart Association. See the chart below.
Note: A diagnosis of high blood pressure must be confirmed with a
medical professional. A doctor should also evaluate any unusually low blood pressure readings.
Medical Marijuana and Healthcare Providers- Part 3 of What’s all of the Fuss about this Marijuana Stuff?
Healthcare providers and legal issues of medical certification
In part 1, I reviewed a brief history of marijuana, discussed medical-grade cannabis, presented some basic information regarding the constituents in the marijuana plant, and gave an overview of the endocannabinoid system. In part 2, I discussed medical marijuana education and information regarding its uses, side effects, and dosing. In the final part of this series, I will discuss information that is specific to healthcare providers in relation to their advocacy role, ethical and legal considerations of the patient that is a healthcare provider, and a review of the current laws/regulations. This information is helpful to both patient/caregiver and medical provider(s).
Continue reading “Medical Marijuana and Healthcare Providers- Part 3 of What’s all of the Fuss about this Marijuana Stuff?”Part 2: What’s all the fuss about this marijuana stuff?

In part 1, I reviewed a brief history of marijuana, discussed medical-grade cannabis, presented some basic information regarding the constituents in the marijuana plant. I apologize in advance for the length of this email! But it is packed full of great information!
In part 2, I will present medical information regarding marijuana and its uses. This information is helpful to both patient/caregiver and medical provider(s) alike. Not only is it important for patients to fully understand how to choose, dose, and utilize their medicine, but it is imperative for providers to begin to have some basic education to help patients make choices about their medications.
Patients need to understand how their medication works and how to use it safely, but also know the effects, side effects and hazards. Some of the known effects of THC (i.e., the psychoactive effects or getting “high”/intoxication) include affecting a person’s memory, cause pleasure or a sense of well-being, alter the sense of time, heightens the senses, affects thinking, concentration, and coordination, according to NIDA.
The effects of the THC component are dosage-dependent. THC is known to be biphasic in its effects. What this means is at lower dosages, patients may experience relief symptoms, but at high dosages, they may experience exacerbated symptoms.
For example, if a patient takes 1 serving of a chocolate bar, they may experience relaxation and decreased anxiety. However, a product 2 or 3 times stronger may cause the same patient to experience heightened anxiety or even panic attacks.
It is possible to have a patient’s environment or situation affect their “high” making it a positive or negative experience. There have been subjective reports of increased appetite, intensified self-awareness, relaxation, euphoria, enhanced creativity, and changes in sexual desire with THC use (Clark, C.S. (n.d.).
CBD has the non-intoxicating (i.e, non-psychoactive) effects of sedation, anti-anxiety, and antidepressant on the brain. In the body, CBD has other effects such as antioxidant, anti-inflammatory, anti-spasmodic, anti-proliferative, analgesic, neuroprotective, anti-psychotic, anti-emetic (anti-nausea) (Leafly, 2017).
The side effects of THC and CBD are also known (Theisen, E. (n.d.):
Many of these side effects can be dosage-related (i.e., the higher the dose the stronger or more side effects a patient may experience). The discussion of side effects also has an unusual twist in relation to THC and CBD. It is known that CBD does have antagonistic effects on the receptors of THC. This means it is possible to use CBD to mitigate or decrease the side effects of THC.
Being aware of the hazards of marijuana use is just as important. Marijuana does affect concentration and motor skills. It’s dangerous to drive or operate heavy machinery while you’re high. Because marijuana impairs short-term memory and judgment and distorts perception, it can impair performance in school or at home/work (NIDA). Whether patients smoke cannabis or eat it, using it with alcohol can heighten alcohol’s effects on the body – thus increasing alcohol and marijuana-related issues or dangers.
Marijuana (CBD specifically) can interact with medications. By its effects on the liver’s enzyme pathways for medications, CBD can increase or decrease the blood levels of some drugs. For example, it can increase the blood levels of blood thinners or make some antiviral drugs not work as well.
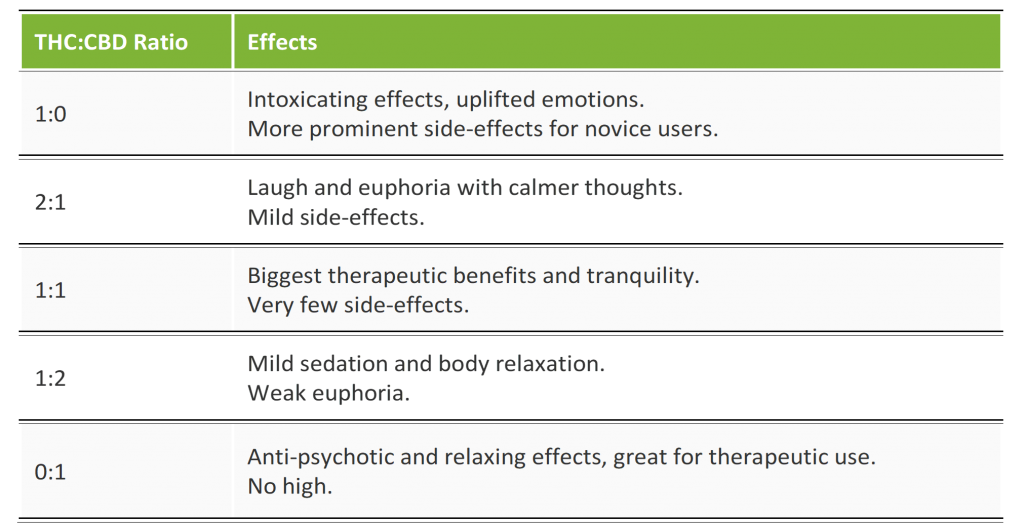
Knowing the effects and side effects of both THC and CBD in one product also helps to provide some guidance in choosing a product. By being able to read a product’s label, patients can determine the type of effects and side effects to expect.
The concentration ratios of THC to CBD provide an initial starting point for evaluating the product’s purpose. As can be seen below, the ratios can help guide a new or experienced patient to choose where to begin based on effects and side effects:
· High THC and low CBD percentages — mainly used by recreational users to get really high. The higher the THC percentage, the stronger and longer-lasting the high.
· High CBD and low THC percentages — perfect for medicinal users who want to experience multiple medical effects without getting high or euphoric.
· Equal CBD and THC percentages — quite rare nowadays, but great for consumers who are looking for a minimal high with a strong focus on relieving symptoms (LUKA, 2017).
One additional side effect/adverse effect of chronic daily marijuana use that needs mentioning is a syndrome called Cannabinoid Hyperemesis Syndrome (CHS). This is characterized by cyclic episodes of nausea and vomiting and gastrointestinal pain. Patients will often use frequent hot bathing as a means to reduce or stop the symptoms. This syndrome is most often seen in people that use more than 3 times per day for several years before symptoms start. It is not permanent and is relieved by having a break or holiday from cannabis use.
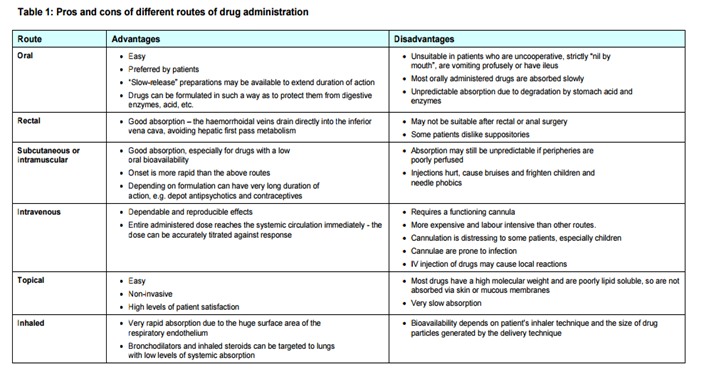
Let’s address the administration, dosage, and route of use. Administration of this medication comes in multiple routes; inhalation/smoking, oral ingestion, and/or topical applications. Understanding the differences between these routes of administration allows for decisions regarding using this medicine. This is important because smoking may be a huge taboo or not recommended due to medical ailments like COPD, but using a topical cream for pain relief may be the ticket!
Additionally, the route does affect the patient’s control of the dosing, and allows for utilizing the most effective routes in the lowest effective dosage, in a safe and manageable way.
Regardless of the route(s) of administration, it is important to understand the results will vary from patient to patient and medication product to product.
Product availability and access to products can vary from dispensary to dispensary and within the same dispensary. Thus, reading labels and understanding how to compare products does guide the patient to be able to discuss their needs with the budtenders at the dispensaries.
Oral/Edible Delivery Methods:
So, let us move our discussion into routes of administration. The oral delivery method has multiple types of products patients can choose from. Products include pills, sublingual (under the tongue) tinctures/oils, sprays, edible/drinkable products like candy or concentrated juice.
Due to the nature of taking these products orally, understand that there is a taste and at times a smell to them. If you are not aware of or cannot tolerate the marijuana taste, this is an important consideration. Many of the newer products are coming up with clever ways to reduce or hide the marijuana flavor. Before you buy an oral product, make sure you can tolerate and/or stomach your choice. Otherwise, you’ve wasted money on medicine you will not use.
In considering what type of oral product, factors to take into consideration include: onset of the medication’s effects, length of time the effects last, and how the medication affects the patient AND side effects to expect.
Oral routes of administration can be difficult to dose due to having to cut/measure the product. They are also known to have the greatest variability of onset times and length of effects within and between products due to production. Because of this variability, I often describe a trial and error process with this route to naïve or new-to-product patients as the “guinea pig process”.
I teach patients the mantra of all medical providers: “Start low and go slow”. What does this mean? Well, for example, let’s consider a medical chocolate bar (see the label of an actual product below). You will notice information listed includes constituent listing in milligrams (mg), the number of servings in the bar, product lot numbers and dates of manufacture and testing, and a disclaimer. See post pictures for the following example.
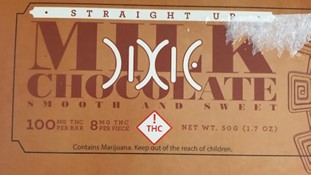
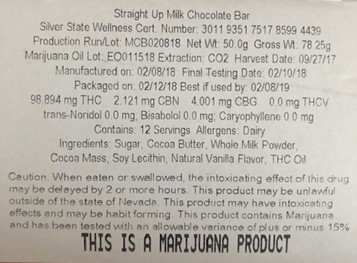
In this example, one serving of this bar is 1 (one) square of the bar and contains 8mg of THC per serving. 8mg of THC to a person that has never used marijuana in any form may be an excessive dose for the first time. It may be so large that the effects are scary or unnerving for the patient. Teaching patients to “START LOW” means starting at the lowest effective dosage.
However, you can begin to see how this may become difficult when it comes to cutting a chocolate bar square into small enough pieces to appropriately dose yourself. In the medical marijuana community, we recommend starting at approximately 2.5mg per serving (especially for naïve patients) up to 10mg/serving.
For the naïve patient and the example chocolate bar product, ¼ of a piece/serving may be a good starting point to trial approximately 2mg. Keep in mind the 2.5mg starting dosage is just a suggestion. I have a patient that finds 2.5mg to be too much and uses more like 0.5mg per dosage. Again, a discussion with the budtender regarding your illness, experience with these products, and desired effects come into play.
The budtenders would never suggest a naïve patient purchase a candy bar that had 100mg/serving, but they won’t stop you from purchasing any products. Good decision-making based on education is key for effective and sustainable self-medicating (Theisen, E. (n.d.).
The “GO SLOW” part of the saying is stated in the caution part of the label. It may take two-plus hours before patients notice any effects AND the effects may last up to 5 (five) hours. Remember, edibles’ effects are often more intense than smoking marijuana.
With this in mind, I instruct patients to wait at least 2 (two) hours prior to administering a repeat dose until the desired effects are obtained. For patients that are more experienced with this form of medication but new to a product, I still encourage them to wait 2 (two) hours then re-dose themselves if the desired effects are not obtained (starting the 2 hour-wait again).
By dosing themselves in stages, patients begin to know their individual lowest effective dose of this medication/product; AND depending upon the lowest effective dose, helps determine if this product appropriate to purchase again.
Determining the lowest effective dosage also helps the patient/caretaker answer other questions such as: What if the product’s lowest effective dose is ½ of the candy bar? Can the patient stomach the flavor of the bar? Can they afford to pay for ½ of a bar for multiple dosages per day over a week or month?
The “start low and go slow” is true for any form of medication. Knowing your individual needed dosage gives you an idea about using products that can be dosed appropriately. But not all products make it easy. Products like lollipops make dosing difficult – again the “guinea pig process” is the only way to know for sure.
Not all oral products take as long to reach effects. Some products can take 15-30min for effective dosing and may be easier to manage. For instance, sublingual tinctures and oral sprays can more easily be dosed per drop/spray and are more economical based on the dosing. Additionally, these faster-acting oral forms may also be a form of breakthrough symptom management to be added to a long-acting edible as prescribed/discussed with your medical provider.
Inhalation/Smoking Delivery Methods:
Marijuana can be inhaled in many ways, including joints, electronic cigarettes, water bongs, hookah pipes, and vaporizers.
When cannabis is inhaled, the gases/smoke enter the lungs and, depending on the type of marijuana and the delivery system, the cannabinoids are absorbed into the bloodstream in varying amounts. Smoking is the quickest way to deliver marijuana into the bloodstream.
Despite hearing how marijuana is “natural”, there is evidence to suggest that marijuana can impair lung function, damage large airway mucosa, and possibly contribute to bullous disease… (Howden & Naughton, 2011). Especially when combined with smoking cigarettes. We do know that in some people (especially those with lung problems), smoking marijuana can make their breathing worse. Marijuana smoke (like tobacco) causes [chronic] coughing, [chronic bronchitis], increased sputum (“phlegm”), and wheezing. Also, marijuana smoke can cause shortness of breath and swelling in your throat. Marijuana smoke may increase your risk of lung cancer.
None of the available delivery devices have been studied in detail to safely say they will protect you from the harmful effects of the smoke. No method of inhalation can therefore be considered [completely] safe. Second-hand smoke (inhalation of another person’s marijuana smoke) can cause serious health problems, especially in infants and children or anyone with a chronic lung condition (ATS, 2017).
Vaporizing is gaining popularity because of its mechanical simplicity and ease of use. Vaporizing uses either dried ground marijuana flower or a liquid/wax-like concentrated marijuana extract. Vaping pens or sticks are a better alternative for health-conscious consumers because they do not combust the medication. Instead of heating the concentrate to a lower temperature, the plant constituents are evaporated into the released vapor.
There is a vast difference in the quality of smoke between smoking and vaping. “When one smokes a joint, or hits their bong, over 75% of the combusted smoke gases contain non-cannabinoid elements, most of which do not get you high and add to the potential health risks. Instead, when one uses a marijuana vaporizer the smoke/gases that they are inhaling consists of approximately 95% cannabinoids…. While leaving behind the toxic and irritating compounds that are simply not needed” (Oranje Pharma, n.d.).
Although vaping is not completely harmless, it is less harsh on the lungs and provides a smoother smoking experience. “To be clear concentrates tend to be about 60-80% THC while the average dry herb is only 10-25% THC” (Hobson, 2018). Thus, using concentrates, patients need less per dose due to increase cannabinoid concentration.
Some of the advantages of using concentrate vaporizers include being more cost-effective since less material needs to be vaped; easier to dose based on the size of inhalation and length of time the vapor and the breath are held (increased diffusion from the lungs into the bloodstream), and there are observations that the vapor is cleaner and less harsh physically in the lungs.
“Another advantage of vaporizers is the efficiency of converting plant matter into active cannabinoids. A collaborative study conducted by California NORML and MAPS found that vaporizers could convert 46% of available THC into vapor, whereas the average marijuana joint converted less than 25% of THC. Likewise, patients ranked vaporizers as the most efficient method of marijuana intake – requiring a lower dose than smoking, edibles, and tea – in a recent study published in the Journal of Psychoactive Drugs” (Oranje Pharma, n.d.).
Regardless of the type of inhalation delivery method used, this is the fastest and easiest way to deliver medication in an easy-to-dose method. The onset for effects takes from 5-15 minutes and may last 2-3 hours (Theisen, E. (n.d.).
As with all administration forms of this medicine, always start at a low dose and go slow to find the most effective lowest dose. If you are unsure what dosage of concentrate to purchase, speak with your budtender about what product is right for you.
Finding the right inhalation product requires trial and error, (i.e., the guinea pig process). So, don’t be dissuaded if the product purchased isn’t the right one; just try another. I have one patient that uses 3 different types of concentrate vaporizers to obtain the greatest amount of relief. This patient had to trial and error multiple products before they found the correct combination.
Topical Delivery Methods:
When looking into topical delivery methods, patients and providers have reasons to appreciate this category. Topical cannabis products are available in salves, lotions, creams, bath salts, balms, and oils. Other forms include transdermal patches or vaginal/rectal suppositories. “They work by being absorbed through the skin [or mucous membranes/intestinal walls), where they activate cannabinoid receptors.
Topical applications are one of the most effective pain treatments available for people with aching joints or muscles who aren’t looking to get high since the THC doesn’t actually enter the bloodstream. This also makes the pain relief properties especially fast because it is applied and absorbed directly by the painful area” (Cannabis Training University, 2018).
While topical products primarily affect pain, they also help with inflammation. Pain, however, is the main use for these products. When choosing a topical product, consider how the different types of products work. The Cannabis Training University (2018) provided a nice summary of various topical options and the best ways to use them.
A salve is a great option for intense pain relief: it’s easy, convenient, relatively mess-free, and absorbs quickly.
Lotion is a better choice for less intense or more general pain. It is less concentrated than a salve or balm, so it will spread over larger areas of skin easier and faster. The lotion also typically includes many moisturizing ingredients to leave your skin feeling smooth and soft.
Oils are perfect for fast relief in areas like feet or elbows with rough skin. Oils also make for a great medicated massage on a painful area.
Lip balms are available and usually include ingredients that will help heal chapped lips. Check out options with peppermint or other scents and flavors for the best results.
Bath salts are one of the most innovative topical products. It can be used for all-over pain relief – just add them to a hot bath. They are also useful for relaxation and deeper, more restful sleep.
Transdermal Patches are designed for systemic (primarily) and local effects. Patches are a way to provide a longer duration of the medication based on the rate it is absorbed through the skin. Patients use these to manage many conditions such as chronic pain, muscle spasms, inflammation, and sports injuries. In 2017, the National Academies of Sciences report supported patients’ claims of pain relief, saying that there is significant evidence that THC can effectively reduce pain and spasms. Patches generally do not cause the “high or euphoria” associated with other routes of delivery. Finally, patches can be quite pricey, averaging $15-20 per patch. The price can vary from brand to brand, and even from dispensary to dispensary, so check with the local dispensaries near you.
Vaginal/Rectal oils/suppositories are cannabis-infused products intended to maximize the muscle relaxing and pain-relieving properties without inducing a psychotropic high. The cannabinoids are absorbed through the vaginal/rectal mucosa due to the rich supply of blood vessels and lymphatics in the intestinal tract.
Regardless of the form of topical product delivery method you choose, the onset times for this route is 10-20 minutes. Patches can last 6-12 hours, whereas suppository effects can last up to 8 hours. Topical lotions/creams/oils have a duration of 2-3 hours. All types of cannabis topicals come in different strengths, so try out a few different options to find one that works the best. (420Evaluationsonline.com, 2016)
Whenever any of my patients are using any new medication or supplement, I instruct patients to be and remain in a safe environment with trusted people/caretakers (for naïve patients) for a day to trial their new medication. A supportive, safe, and positive environment to experiment with this medication does impact the results.
Naïve patients may experience medication effects and/or side effects that may cause anxiety or distress. Having trusted people around to help monitor and calm a high, anxious person can be very helpful. This process should be repeated with any new product regardless of the patient’s previous experience.
It is helpful to understand that if too much of this medication is administered, the patient will not die. There have been no reported cases of death by overdose from marijuana alone. However, an accidental/unsuspected elevated dosage may cause an experience for the patient that dissuades the use of this medication again. Teaching patients to find the lowest effective dosage, and how to evaluate how the medication affects and side effects aids patients in becoming active participants in their care.
Common dosing and use questions:
– How much should I use?
· Ratios and dosage depend on condition. Some require a higher CBD-to-THC ratio.
· Less is more as we have seen with the biphasic aspect of THC’s effects.
· Start low and slow and titrate up.
– How often should I dose?
· Depends. In general, THC can be dosed at night before bed to minimize side effects and CBD can be dosed throughout the day. Patients can benefit from multiple different delivery methods throughout the day/night depending upon their condition and desired effects of the medication.
– How long do I have to take this medication?
· Can be long-term depending on what’s being treated. Cannabis is not a silver bullet and requires patience and diligence. (Theisen, E. (n.d.).
– What about tolerance development? Won’t I keep needing more medicine?
· Tolerance to cannabis develops more slowly than tolerance to heroin, nicotine, alcohol, or cocaine. But is still develops. Patients using the lowest effective dosage may have to increase their dosage if needed over time. Taking a drug holiday away from marijuana use may help with tolerance issues. Talk with your medical provider regarding this.
– What about abuse or addiction to marijuana?
· The National Institute on Drug Abuse reported on studies that suggest 30 percent of those who use marijuana may have some degree of “marijuana use disorder”. The researchers report the use disorder can morph into an addiction when the person can’t stop using the drug even when it interferes with their daily activities. (NIDA, 2018). If you believe you are having issues with use, abuse or addiction issues, please contact your medical provider for assistance.
– What about micro-dosing marijuana?
· Micro-dosing is all about using smaller amounts of marijuana throughout the day to potentiate the medicinal properties without getting stoned/high. This mode of cannabis intake has several benefits: cost-effective and helpful for controlling unwanted side effects of marijuana.
Micro-dosing has been shown to be more effective for ailments such as neuropathic pain, according to a study conducted by the Medicinal Cannabis Research Center at the University of California. Micro-dosing is using 2.5mg of cannabis throughout the day to allow for patients to function properly around others without looking/acting stoned or inebriated (Smith, 2016).
– What dose of marijuana is considered equivalent to an opiate?
· Patients are often using marijuana for pain management, either as an adjunct to current pain management therapies or as solitary treatment. Knowing marijuana does enhance opiate effects is important. It is reported that 5mg of THC is equivalent to 30mg of codeine (Wolski, K. (n.d.). Studies are showing that cannabis use in combination with opioids for pain management enables patients to decrease and eventually stop the opioids.
– What does green testing mean?
· Patients in the dispensary can talk with their budtender about the quality of their medicinal product. Patients need to ask and ensure products are green tested – testing by the laboratory of the product to help ensure the lack of pesticides, fungicides, herbicides, heavy metals, or other contaminants in their medicine. Don’t be afraid to ask to see the reports. All quality products should have this information available (Wolski, K. (n.d.).
References:
American Thoracic Society (ATS). (2017). Smoking Marijuana and the Lungs. Am Journal Respiratory Critical Care Med. 195: P5-6. https://www.thoracic.org/patients/patient-resources/resources/marijuana.pdf
Cannabis Training University. (2018). Cannabis Topical Types. Retrieved from https://cannabistraininguniversity.com/cannabis-topical-types/
Clark, C.S. (n.d.). The Endocannabinoid System, Online Course viewed 12/12/18. The Medical Cannabis Institute.
Hobson, J. (2018, Apr. 11). Concentrate vs. Dry Herb Vaporizers: What’s Better? Herb.com @ https://herb.co/news/health/dry-herb-vs-concentrate-vaporizers/
Howden, M.L. & Naughton, M.T. (2011). Pulmonary Effects of Marijuana Inhalation. Expert Rev Resp Med. 5(1):87-92. https://www.medscape.com/viewarticle/738255
Leafly. (2017, Feb). Cannabis 101. Maximizing CBD’s Effects and Benefits: 5 Experts Weigh In. https://www.leafly.com/news/cannabis-101/cbd-effects-benefits-whole-plant-medicine
LUKA. (2017, May 8). THC vs CBD: Effects and Benefits (Backed by Science). https://greencamp.com/thc-vs-cbd/
NIDA. (2018, June 25). Marijuana. Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana on 2019, January 6
National Institute of Drug Abuse (NIDA). Marijuana. Retrieved from https://www.drugabuse.gov/drugs-abuse/marijuana on 2019, January 5.
Oranje Pharma. (n.d.). Smoking Marijuana vs. Vaporizing Marijuana. Retrieved from https://420vapejuice.ca/smoking-marijuana-vs-vaporizing-marijuana/
Smith, D. (2016, Jul. 22). The Art of Marijuana Microdosing. What is Microdosing Cannabis and How Do You Do It? Retrieved from https://cannabis.net/blog/medical/the-art-of-marijuana-microdosing
Theisen, E. (n.d.). The Endocannabinoid System, Online Course viewed 12/12/18. The Medical Cannabis Institute.
Wolski, K. (n.d.). Cannabis Prohibition: The Harmful Consequences, Online Course viewed 12/12/18. The Medical Cannabis Institute.
What’s all the fuss about this marijuana stuff? Part 1 of 3

As a healthcare provider, a patient, a family member and loved one, I try to view all sides of how a person decides to treat, heal or cure an ailment. If the treatment is effective with minimal to no side effects, then it is hailed a success; even if the real success was more attributable to the innate healing nature of the patient’s body.
Thankfully science definitely plays a role in the identification of assistive and supportive measures found in medicine of all types and philosophies. It is important to understand the majority of interventions of healthcare are really meant to be supportive of the body’s innate healing. Things like medications, healthy lifestyle choices, and stress management are meant to help support and maintain the body’s balance of homeostasis.
As a healthcare provider, it is important that my decisions and recommendations of care to my patients is based in science and also driven by the patient’s beliefs and definitions of what health and wellness are.
Continue reading “What’s all the fuss about this marijuana stuff? Part 1 of 3”Cold Laser Therapy
“I’ve tried various prescriptions for this pain. How can a laser help?” Often I am confronted with this and other similar questions regarding post-herpetic neuralgia (PHN) and other types of nerve pain. I have had the pleasure of seeing patients’ smiling faces when they begin having a decrease and/or resolution of nerve pain.
Continue reading “Cold Laser Therapy”Is your life all work and no play?
Is your life all work and no play? When was the last time you did something enjoyable just for yourself? Spent the day relaxing comfortably all alone? Or spent quality 1 on 1 time with a close friend content in just being together, talking, walking, wondering about life in general? When did you last spend time reflecting on the spiritual aspect of your life, sitting in meditation or prayer, or just looking up at the stars in wonder?
Continue reading “Is your life all work and no play?”Yoga thru the Years by Susan Fritz
As this is my first time on this blog, let me introduce myself. I am affectionately called SierraSue by friends because of my love for nature. I am a natural kind of woman and perhaps that is the reason I was drawn to Yoga so many years ago. This blog will be about my journey with yoga through the years.
Continue reading “Yoga thru the Years by Susan Fritz”Dealing with Insurance Hurdles
I came across this pdf flyer regarding insurance issues and suggestions of how to work through them. This was put together by the Patient Advocate Organization. Click the link below. It is written in a easy to read brief that there is little for me to add! Great resource in the time of trying insurance issues that change year to year.
Healthcare Provider-Patient Communication
One of the biggest complaints I continue to hear from patients and clients is the issue of lack of communication with their healthcare provider, most notably physicians and mid-level providers. Communication issues seem to be related to a few categories including: inattention to the patient (various reasons), lack of empathy and/or big picture of the patient, lack of time, unacceptance of alternative health approaches by the patient, and generational views of the healthcare provider by the patient.
Continue reading “Healthcare Provider-Patient Communication”